Campylobacter In DogsUpdated 7 months ago
A common cause of foodborne illness in humans after consuming contaminated undercooked meat or unwashed vegetables, “Campy,” is also a concern for dogs who may get diarrhea from the infection and then shed these bacteria in their stools.
My Dog Tested Positive For Campylobacter
MySimplePetLab Routine Dog Stool Test with PCR Upgrade includes PCR assay tests for disease-causing bacteria, viruses, and protozoa found in dog intestines. One of those bacteria is Campylobacter. A positive test means Campylobacter DNA was detected in the stool. Most veterinarians then assume the dog is infected with Campylobacter (called Campylobacteriosis) and shedding the bacteria in the stool.
However, your dog may not need treatment because this finding is not always associated with symptoms of illness. Most dogs infected with Campy will quickly suppress the parasite and never get sick or only have mild symptoms. Positive dogs may shed Campy occasionally or frequently so good hygiene practices and risk to family health from these bacteria should be reviewed.
A test result is not the same as a veterinarian’s diagnosis, so it’s always best to consult with a veterinarian about your dog’s test results to determine the safest and most effective treatment and prevention plan, and when to do follow-up stool tests. If treated, most veterinarians will recommend rechecking a dog’s stool sample within 2-4 weeks after treatment for Campy. If you have other pets (dogs or cats) in the household, consider testing them as well since Campy in one pet can often lead to Campy in others.
It’s important to know that some dogs will continue to test positive for Campy for an unknown period after treatment. This is most likely because the dog remains in an environment where re-infection keeps occurring, but not always. Other considerations for treatment failure are poor immune response and drug resistance.[6]
MySimplePetLab Routine Dog Stool Test include a reference lab stool O&P (fecal ova and parasites) which screens for roundworms, hookworms, tapeworms, whipworms, and some types of coccidia. Bacteria (including Campylobacter) are not visible on this type of test which is why PCR testing (MySimplePetLab Routine Dog Stool Test with PCR Upgrade) is needed.
Please consult your healthcare professionals if you are pregnant, immune-compromised, or have any concern about the risk of Campylobacteriosis.
My Dog Tested Negative For Campylobacter
MySimplePetLab Routine Dog Stool Test with PCR Upgrade includes PCR assay tests for disease-causing bacteria, viruses, and protozoa found in dog intestines. One of those bacteria is Campylobacter. A negative test means Campylobacter DNA was not detected in the stool, which is great news. No one wants their dog or puppy shedding these bacteria and maybe putting other pets or people at risk of infection.
Depending on their lifestyle, dogs can remain at risk of Campy exposure so a negative test result today doesn’t mean it couldn’t be positive later. Since dogs may shed these bacteria occasionally, it’s possible to test a stool sample from an infected dog without any of this parasite’s DNA. This is called a “false negative” when the test result is negative, but the dog is infected.
If Campy infection was suspected and you have other pets in the household, consider testing them as well since Campy in one pet can often lead to Campy in others. Dogs negative on Campylobacter by PCR but still with Campy-like symptoms such as abnormal stools, likely have a different explanation for the symptoms. Please consult with a veterinarian if this is the situation with your dog.
Learn More About Campylobacter
What Are Campylobacter?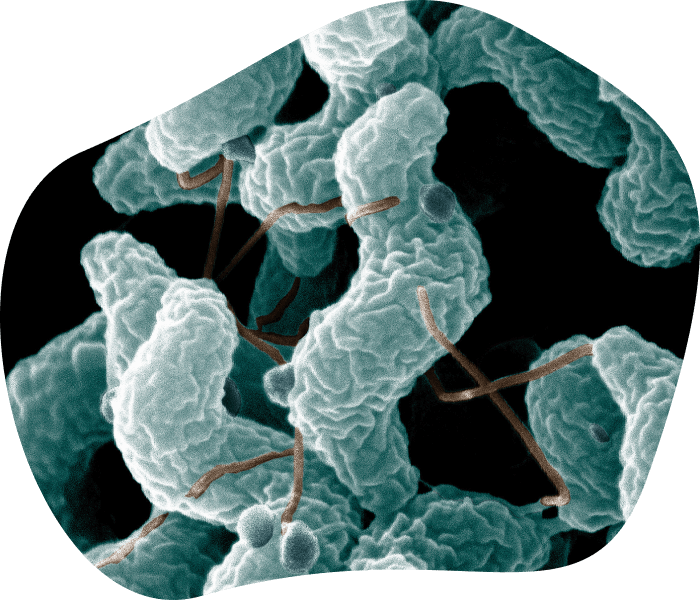
Campylobacter spp. (species) are microscopic bacteria so cannot be seen by the naked eye. They are a major cause of foodborne illness in humans and pets around the world.[3,4]
Campy infects dogs, cats, people, and other animals including pigs, poultry, cattle, sheep, rodents, and ferrets.[4] Some types of Campy prefer certain animal hosts (C. lari infects dogs; C. helveticus infects cats) while others can be harmful to more than one kind of animal (C. jejuni, C. coli and C. upsaliensis in dogs, cats, and people).[4,6]Campylobacter jejuni is by far the most common type associated with diarrhea in dogs, cats, and people, and transmissible between them.[4,6]
Campy belong to a large family of Gram-negative bacteria called Campylobacteraceae which also includes the Helicobacters. Helicobacter pylori is well-known in humans for causing stomach discomfort, ulcers, and even cancer. Helicobacters are also common stomach bacteria of dogs and cats but are unlikely to cause illness in pets. Campylobacters are intestinal parasites but, in some circumstances, will migrate into the bloodstream (septicemia) or organs to cause more widespread illness in the animal or human.[3,6]
A common source of Campylobacter infection for pets is being fed uncooked or unprocessed foods.[3,6] Even if pet owners are not feeding raw foods, dogs can get infected with Campy from eating animal stool or things contaminated by the stool (water, soil, grass, plants). Fortunately, Campy doesn’t usually make dogs sick.[4] Many dogs can carry and shed these bacteria into their stool without any signs of illness. This ongoing or occasional shedding can lead to infecting other pets or people through direct physical contact or indirectly from stool contamination.
People also can get infected by accidently consuming food or water that was contaminated with Campy from human or animal stool.[5] A common human source of infection is raw meat (especially poultry) sold in the U.S. for consumption by people or animals.[6]
How Common Is Campylobacter?
Campylobacter infection is one of the most common causes of digestive upset in people around the world, and the most common bacterial causes of diarrhea.[3] Campylobacter also infects dogs, cats, and other animals including pigs, poultry, cattle, sheep, rodents, and ferrets.[4] Some types of Campy prefer certain animal hosts while others can be harmful to more than one kind of animal.[4]Campylobacter jejuni (the most common type associated with diarrhea in dogs, cats, and humans) and Campylobacter coli are both transmissible between pets and people. They can both cause disease in both humans and animals.[4,6]
C. jejuni has been detected in 29% of dogs with diarrhea and 21% of cats with diarrhea.[6] However, results of studies examining the frequency of Campy infections in dogs and cats with and without diarrhea vary widely from 0% to 50%.[6] These percentages are interesting but less important than the risk factors of individual pets and families.
Fortunately, Campylobacter doesn’t usually make dogs sick.[4,6] Many dogs can carry and shed these bacteria into their stool without any signs of illness. Most dogs infected with Campylobacter jejuni or C. coli become healthy carriers of the bacteria but may shed Campy in their stool occasionally or frequently. This represents a leading source of contamination for other dogs, cats, and people.[3,5,6]
People get infected more commonly by accidently consuming food, milk, or water that was contaminated with Campy from human or animal stool.[3,5] A common human source of infection is raw or undercooked meat sold in the U.S. for consumption by people or animals.[3,5,6] Contaminated chicken or foods that came in contact with contaminated chicken (salad, fruit, vegetables) are the most common cause of infection in people.[3,5,6]
Campylobacter can survive for long periods of time in stool, urine, water, and milk, especially in cold temperatures that are above freezing.[4] Dogs may ingest the bacteria from contaminated water sources or when eating stool from other dogs or animals (rodents, livestock, poultry) while in the backyard, out for walks, in dog parks, etc. One dog can spread Campy to other dog (and cat) housemates or be exposed to contaminated stool when housed with other dogs like kennels, day cares, or shelters.[1,2]
What Does Campylobacter Look Like?
Campylobacter spp. are motile with a single or double tail (flagellum) that helps them move. They are slender, curved rods (called bacilli) and not circle-shaped (called cocci) or spiral-shaped (called spirochetes). None are seen by the naked eye but under the microscope look comma-shaped or gull-wing-shaped.[4,6]
Campy belong to a large family of Gram-negative bacteria called Campylobacteraceae which also includes the Helicobacters. Helicobacter pylori is well-known in humans for causing stomach discomfort, ulcers, and even cancer. Helicobacters are also common stomach bacteria of dogs and cats but are unlikely to cause illness in pets.
Gram staining is a classic benchtop method for distinguishing types of bacteria in a sample (Gram negative versus Gram positive), staining them either pink (negative) or purple (positive) on a microscope slide. Campylobacter stain faintly pink (Gram negative) with this method.[4,6]
Bacteria are not visible on a standard fecal O&P (ova (egg) and parasite) stool test. The O&P looks for worms and some types of coccidia, not bacteria. While Gram staining stool (fecal smear) can be helpful when searching for a bacterial cause of abnormal stools (diarrhea), the specific type of bacteria like Campylobacter cannot be reliably identified in this way. Most of the time, a special Polymerase Chain Reaction (PCR) test is used to detect the presence of this parasite in dog stool (MySimplePetLab Routine Dog Stool Test with PCR Upgrade).
What Symptoms Are Caused By Campylobacter?
Fortunately, Campylobacter doesn’t usually make dogs sick.[4,6] Many dogs can carry and shed these bacteria into their stool without any signs of illness. This ongoing or occasional shedding can lead to infecting other pets or people through direct physical contact or indirectly from stool contamination.
Dogs are more likely to get sick from Campy if they are puppies younger than six months of age.[4,6] Stress from overcrowding, other simultaneous infections (like Giardia, Salmonella, or dog coronavirus), and a weakened immune system are all risk factors for Campylobacteriosis (disease from Campylobacter).[6] Ingesting a large concentration (number) of Campy can increase the number of bacteria that survive passing through the acid of the stomach, increasing the risk of illness.[6]
Dogs sick from Campy usually have signs of digestive upset, most commonly loose stool or watery diarrhea (which may be bloody, with mucus, or with bile) with or without vomiting, loss of appetite, abdomen pain, decreased energy level, and fever.[2,4] The diarrhea may come and go and may last for weeks.[1,6] Rarely, severe symptoms like electrolyte imbalances, vomiting that won’t stop, shock and even death can result if Campy gets into the dog’s bloodstream or organs
For people, illness usually appears 2 to 5 days after infection.[3,5] Symptoms include fever, abdominal pain (cramps), diarrhea (often bloody), nausea and vomiting lasting 1 to 10 days.[3,5] Most people will recover without treatment.
How Do Dogs Get Campylobacter?
Campylobacter can survive for long periods of time in stool, urine, water, and milk, especially in cold temperatures that are above freezing.[4] In adverse conditions, C. jejuni can convert to a dormant form that can reactivate when ingested.[4] Stool from dogs and other animals shedding the bacteria can contaminate water sources frequented by pets. Dogs may also ingest the bacteria when eating stool from other dogs or animals (rodents, livestock, poultry) while in the backyard, out for walks, in dog parks, etc. One dog can spread Campy to other dog (and cat) housemates or be exposed to contaminated stool when housed with other dogs like kennels, day cares, or shelters.[1,2]
Campylobacter jejuni (the most common type associated with diarrhea) is easily transferred between pets and people and causes disease in both humans and animals.[4,6]Campy can contaminate raw food or treats, with raw or undercooked meat (swine, cattle, turkeys, horses, chicken, turkey, fish, shellfish) being a major risk factor for infection.[3,4] Uncooked or unprocessed foods also pose an increased risk to the humans handling it. Surfaces exposed to the contaminated food like food dishes and countertops for raw meat preparation also represent a human and pet infection risk. In people, 50-70% of infections come from chicken. Unpasteurized milk is also a well-documented source.[4,6]
Puppies less than 6 months old that contract Campy are at much higher risk for illness compared to adult dogs, with diarrhea commonly lasting 5-15 days.[4]
What Is The Campylobacter Lifecycle?
Dogs can ingest Campylobacter from eating contaminated food or treats (uncooked or unprocessed) or animal stool, or ingesting water, soil, or vegetation (grass, plants) contaminated from stool (fecal material) in the environment.
A high concentration (number) of Campylobacter bacteria ingested increases the dog’s risk of getting sick.[4,6] This is because a large portion are destroyed by the acid of the stomach.[4] The bacteria that get through infect the cellular lining of the small and large intestines. Within days this can lead to inflammation and swelling of the intestinal cells and local lymph nodes, and damage to the hair-like covering (microvillous) of the digestive tract lining. The infection can cause ulcers of the intestines and even bleeding into the stool.[4,6]
Beyond invading the cells of the intestines, Campy can release damaging toxins (cytotoxins, enterotoxins).[4,6] In severe cases, Campy can also enter the bloodstream (bacteremia) and get spread throughout the body, causing widespread inflammation and toxin release.[4,6] These more severe infections can lead to fever, toxic shock, and even death.
After initial infection, the timing and frequency of shedding of Campy into the stool isn’t well understood. Most dogs become healthy carriers of the bacteria while others can get abnormal stools (watery, mucous, or bloody diarrhea) or quite sick. Shedding of Campy in stool can potentially be ongoing or occasional, presumably reactivated later with stress, overcrowding, weakened immune system, or other infections. It is known that Campy shedding can persist for long periods of time and occur in both dogs with diarrhea and healthy dogs with normal stools.[6]
Campylobacter infects dogs, cats, people, and other animals including pigs, poultry, cattle, sheep, rodents, and ferrets.[4] Some types of Campy prefer certain animal hosts while others can be harmful to more than one kind of animal.[4]Campylobacter jejuni (the most common type associated with diarrhea in dogs, cats, and people) and Campylobacter coli are both transmissible between pets and people. They can both cause disease in both humans and animals.[4,6]
Can People Or Other Pets Get Campylobacter?
Yes. Campylobacter infection is one of the most common causes of digestive upset in people around the world, and the most common bacterial causes of diarrhea.[3]
Campylobacter infects dogs, cats, people, and other animals including pigs, poultry, cattle, sheep, rodents, and ferrets.[4] Some types of Campy prefer certain animal hosts while others can be harmful to more than one kind of animal.[4]Campylobacter jejuni (the most common type associated with diarrhea in dogs, cats, and humans) and Campylobacter coli are both transmissible between pets and people. They can both cause disease in both humans and animals.[4,6]
People get infected by accidently consuming food, milk, or water that was contaminated with Campy from human or animal stool.[3,5] Milk can get contaminated when a cow’s udder has a Campy infection or gets manure with Campy on the udder. Pasteurization (heating long enough to kill illness-causing germs) makes milk safe to drink.[3] A common human source of infection is raw or undercooked meat (swine, cattle, turkeys, horses, chicken, turkey, fish, shellfish) sold in the U.S. for consumption by people or animals.[3,5,6] Contaminated chicken or foods that came in contact with contaminated chicken (salad, fruit, vegetables) are the most common cause of infection in people.[3,5,6] Surfaces exposed to the contaminated food like food dishes, cutting boards, and countertops for raw meat preparation also represent a human infection risk.
For people, the infectious dose of Campy can be just a few hundred bacteria.[6] Illness usually appears 2 to 5 days after infection.[3,5] Symptoms include fever, abdominal pain (cramps), diarrhea (often bloody), nausea and vomiting lasting 1 to 10 days.[3,5] Most people will recover without treatment. Very young children, the elderly, and people with weakened immune systems (e.g., HIV, during chemotherapy, illness) are at higher risk of more severe infections.[5]
Most dogs infected with Campylobacter jejuni or C. coli become healthy carriers of the bacteria but may shed Campy in their stool occasionally or frequently. This represents a leading source of contamination for other dogs, cats, and people.[3,5,6]
How Is Campylobacter Prevented And Treated?
Feeding commercially available heat-processed dog food helps avoid Campylobacter infection compared to raw or unprocessed diets. Meat should be thoroughly cooked (poultry to over 165 degrees Fahrenheit) and meat pasteurized.[3] Good handling sanitation and storage of dog food is important, especially with raw food diets.
Pet owners feeding raw or unprocessed foods to their dog should consider health risks to the pet and family. 1) Since a high percentage of raw meat purchased for people or pets in the U.S. is contaminated with Campylobacter, home surfaces like countertops for raw meat preparation and pet food dishes will represent a daily human infection risk. 2) Campy is a Gram-negative pathogen with a tendency to develop multi-drug resistance (MDR) to antibiotics. The Campy on the raw food might already have MDR, and these bacteria can be shared between pets and the human family. 3) Most dogs can be healthy carriers of Campy while shedding the bacteria in their stool, but some dogs and puppies can get quite ill. 4) Some human family members like children under 5 years old, the elderly, or those with weakened immune function are at much higher risk of illness from Campy. 5) It can be difficult to eradicate once in the environment.
Even if pet owners are not feeding raw or unprocessed foods, dogs may ingest the bacteria when eating stool (on soil, grass, plants) from other dogs or animals (rodents, livestock, poultry) while in the backyard, out for walks, in dog parks, etc. Campy can last for extended periods of time outdoors and indoors. Cages in hospitals, kennels, and shelters should be cleaned and disinfected routinely. Household bleach (diluted 1:32, or 4 oz per gallon of water) can be used as a surface disinfectant after cleaning and allowed to fully dry before reintroducing pets to the area.
Treatment is based on the severity of symptoms. Antibiotic therapy is not recommended for dogs who have no symptoms or mild signs that respond to supportive therapy like hydration, rest, and digestive support. This is because of Campy’s tendency for multi-drug resistance (MDR) and risk of passing this MDR to people. For dogs that require more assertive therapy, some antibiotics like erythromycin can be effective against Campy.[4,6] However, antibiotics should not be given without a veterinarian’s prescription and supervision. In more severe cases, hospitalization, fluid therapy, and other treatments may be required. If your dog is sick, you should contact a veterinarian immediately.
Where Are Campylobacter Medications Purchased?
MySimplePetLab does not dispense or prescribe medications, and there are no FDA-approved medications in the U.S. for Campylobacter treatment. Therapy is based on the severity of symptoms. Antibiotic therapy is not recommended for dogs who have no symptoms or mild signs that respond to supportive therapy like hydration, rest, and digestive support.
For dogs that require more assertive therapy, some antibiotics can be effective against Campylobacters including erythromycin, clindamycin, and some cephalosporins.[1,4,6] However, these should not be given without a veterinarian’s prescription and supervision.
Important: Campylobacters can develop multi-drug resistance (MDR) to antibiotics and then transfer those genes of resistance to Campy of the same type, to Campy of different types, and to other kinds of bacteria.[4,6] Since these bacteria can be shared between pets and people, pressuring Campy with antibiotic treatment can lead to the development of antibiotic resistance (especially if inappropriate selection or administration of antibiotics). This can lead to drug resistant Campy in the pet but potentially also in the human family.
While it is always best to consult with a veterinarian prior to administering any medication, even an OTC version, it is especially true for off-label treatment of Campylobacters given the risk of antibiotic resistance. Always read the medication administration directions carefully and be on the lookout for potential side effects (like vomiting) when any medication is administered.
When/How Is Dog Stool Tested For Campylobacter?
Simply put, include a PCR test for Campylobacter whenever a dog has frequent or ongoing abnormal stools (soft stool or diarrhea) or other digestive problems. Need details? Read on.
MySimplePetLab Routine Dog Stool Test with PCR Upgrade includes a Campylobacter by Polymerase Chain Reaction (PCR) assay along with PCR tests for other disease-causing protozoa, bacteria, and viruses found in dog intestines. These tests are designed to find the DNA of hard to find microbe pathogens. Screen for Campy in dogs with signs of digestive upset, most commonly loose stool or watery diarrhea (which may be bloody, with mucus, or with bile) with or without vomiting, loss of appetite, abdomen pain, decreased energy level, and fever.[2,4]
Most of the time, Campylobacter infections are not discovered unless veterinarians are searching for the cause of diarrhea or other digestive problems in dogs or puppies. Once found, vets may encourage pet owners to test other pets in the same household to determine if they are also shedding Campylobacter.
Veterinarians recommend stool (fecal) testing puppies 2 to 4 times during their first year of life, and 1 to 2 times each year in adult dogs (every 6 to 12 months). Veterinarians often call this stool health test a “Fecal O&P”, with the O&P meaning “ova (eggs) and parasites”. It includes special preparations of the stool sample and analysis using a microscope to look for roundworms, hookworms, tapeworms, whipworms, and some types of coccidia. Bacteria are not visible on a O&P stool test (included in all MySimplePetLab Routine Dog Stool Tests). Most of the time, a microbe by PCR test is used to detect the presence of this parasite in dog stool (MySimplePetLab Routine Dog Stool Test with PCR Upgrade).
Additional Questions? Chat us at MySimplePetLab.com, email [email protected], or call us at 833-PET-TEST (833-738-8378).
Sources
- VCA Hospitals, Campylobacter Infection in Dogs
- PetMD, Bacterial Infection (Campylobacteriosis) in Dogs
- Centers for Disease Control and Prevention, Campylobacter (Campylobacteriosis)
- Merck Veterinary Manual, Overview of Enteric Campylobacteriosis
- World Health Organization
- Greene Infectious Diseases of the Dog and Cat: Campylobacter Infections, 3rd ed. St. Louis, Elsevier Saunders 2006, pp. 339-343
Page Image Source: Wikipedia
